What is Living GREAT for Diabetes
GRoup Empowerment And Training (GREAT) for diabetes is an initiative that works with groups of patients to educate and empower them for self-management and better control of their diabetes as well as training healthcare workers to facilitate these groups. We think about GREAT in terms of its structure, resources and communication style. You can download a brochure here.
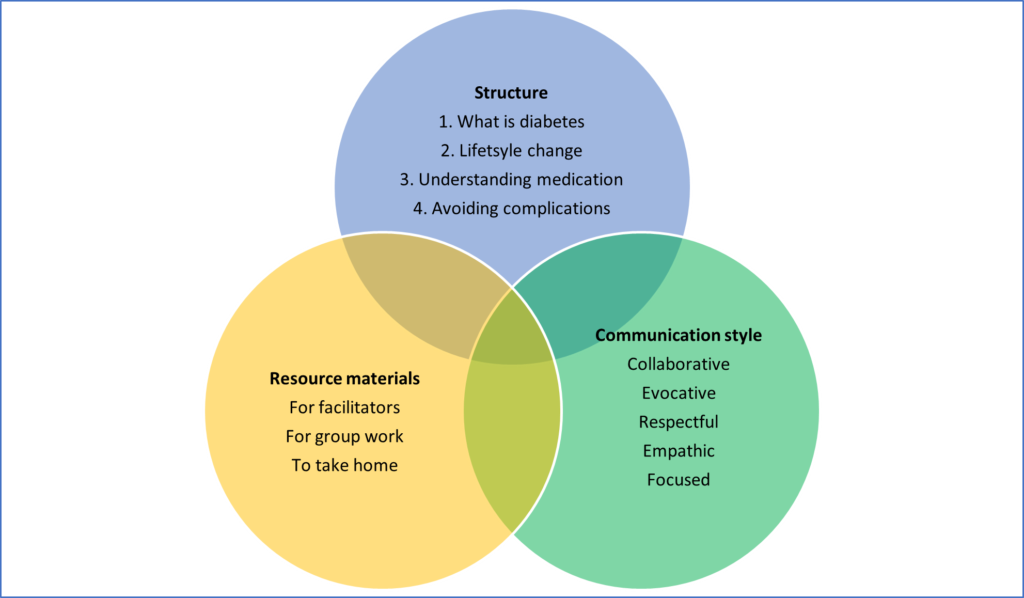
Structure
GREAT consists of 4-5 sessions of 60-120 minutes with 10-15 patients at a time. The four sessions focus on:
- Understanding diabetes
- Lifestyle modification (1-2 sessions)
- Understanding medication
- Avoiding complications
People complete the four sessions and then exit the programme. They can always come back again to refresh themselves in the future.
The group facilitator has typically been a health promotion officer or a professional nurse. The facilitator can involve other healthcare workers such as pharmacists or medical officers if they are available in some of the sessions. In some places, the local dieticians have championed GREAT.
Each session is structured and described in detail in a training manual. An overview of the session content is given below:
Session 1: What is diabetes?
- Introductions and eliciting people’s stories of diabetes.
- A “true/false” game that explores common ideas and misconceptions about diabetes.
- An explanation of what diabetes is using pictures on the flipchart.
- Conclusion that elicits changes in lifestyle as a result of this session.
Session 2: Lifestyle change (this session can also be split into two if necessary):
- Eliciting any changes in lifestyle since the last session.
- Exploring a healthy diet with use of food card pictures (types of food, portion size, timing of meals, ways of cooking)
- Increasing physical activity
- Other lifestyle issues (e.g. alcohol, stress, tobacco smoking)
- Conclusion that elicits changes in lifestyle as a result of this session.
Session 3: Understanding the medication
- Eliciting any changes in lifestyle since the last session.
- Managing diabetes with medication
- Dealing with low blood glucose
- Symptoms of high blood glucose
- Conclusion that elicits changes in lifestyle as a result of this session.
Session 4: Controlling diabetes and avoiding complications
- Eliciting any changes in lifestyle since the last session.
- Understanding complications (including mental health)
- Foot care
- Understanding the clinic and test results
- Closure and setting final goals for lifestyle change.
In Cape Town, GREAT has typically been offered to new patients and those that are not well controlled (HbA1c >10%). These patients usually attend the health centre on a monthly basis and the 4 sessions are offered sequentially on the dates of their planned visits. The sessions are mostly facilitated by health promoters and sometimes nurses, with support from others if available (i.e. pharmacist, dietician). The family physicians have championed the introduction of GREAT as part of their clinical governance responsibilities for diabetes. Patients attend the group sessions usually during the morning when they would be waiting to be seen or waiting for medication. Dispensing is fast-tracked for those that attend GREAT as an incentive to participate.
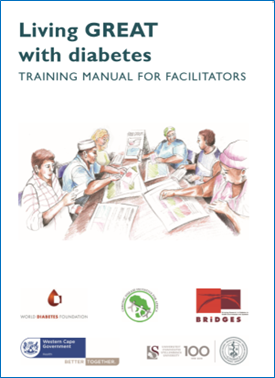
In order to implement GREAT for diabetes in primary care there is a need to train healthcare workers to facilitate the groups of people with diabetes. Training takes between 3-4 days depending on the prior expertise of the participants. The training has to ensure that at the end of the workshop participants (1) know the underlying diabetes content and are confident to apply this content in conversations about diabetes (2) know the structure of the GREAT programme and can confidently use all the resource materials (3) can facilitate GREAT in a patient-centred guiding style (4) can facilitate small group processes, interactions and collaboration.
The educational strategy makes use of the same group-based guiding style. Theory and content are shared using brief talks or through group activities such as the jigsaw technique. Skills and competencies are modelled using either videos or by role play of the group education sessions using the participants as patients. Skills and competencies are acquired by practice with simulation and feedback. Health care workers are provided with a complete set of resources to facilitate the group diabetes education programme.
After the training workshop the facilitators are expected to implement GREAT in their facility with the support of the chronic care team and facility management.
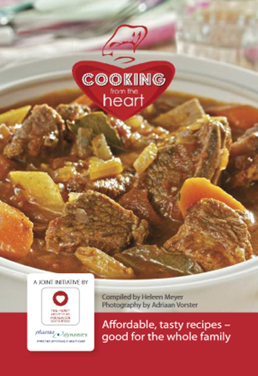
It requires the facilitator to adopt a guiding style derived from motivational interviewing. This guiding style emphasises collaboration and interaction, evoking ideas and solutions from the group rather than telling people what to do, exchanging information rather than just giving information, and respecting people’s viewpoint, choice and self-autonomy. The sessions are supported by a variety of materials that have been developed locally. These include pictures collected together in a flip chart to enable explanation and discussion of what is diabetes and healthy eating, food cards with a wide variety of typical South African foods to assist with discussions about healthy eating, true/false cards with a variety of typical local beliefs and ideas that enable critical discussion and reflection. Patient education leaflets that can be taken home have also been developed in a tabloid format on key lifestyle issues such as healthy eating, physical activity, tobacco smoking, alcohol use and foot care. A South African recipe book and supportive material on type 2 diabetes has also been developed. Many of these resources are available at the ichange4health website.
Communication style
Facilitators are taught a guiding style that is derived from motivational interviewing:
- Collaborative: The people in the group participate in the conversation at least as much as the facilitator. It is a dialogue and not a lecture that engages people in making sense of their condition.
- Evocative: Whenever possible ideas about diabetes and solutions for self-management are evoked from the group members. The facilitator does not tell people what they “must do”, as suggestions from the group are likely to be more feasible and motivating.
- Empathic: The facilitator actively tries to understand the people’s context, concerns and ideas and to engage with active listening.
- Respectful: The facilitator respects the choices and control that people have over their own lives and does not try to coerce people in doing what they are not ready to do.
- Focused: The facilitator keeps the conversation focused on the topic and the group process moving forward. They do not allow the group to deviate to irrelevant topics or unrelated issues.
In order to do this a number of specific communication skills are needed:
- Asking: the ability to consciously use both open and closed questions. The ability to use open questions that encourage elaboration, evocation and empathy is developed.
- Listening: the ability to actively listen through the use of non-verbal and verbal means. Reflective questions, listening statements and summaries are developed.
- Informing: the ability to inform in a cyclical and collaborative manner using the technique of elicit-provide-elicit. In fact each session is designed around the principles of elicit-provide-elicit.
In addition, attention is paid to managing groups. For example, dealing with quiet or over talkative people or handling conflict.
Resource materials
For the facilitator
Three resources are provided to ensure sufficient knowledge of diabetes and of how to facilitate the sessions.

For the group sessions
A variety of resources help to stimulate engagement and collaboration. These include a number of pictures in a flipchart and a number of card games as well as handouts.

To take home
Patient educational materials to take home can reinforce learning and motivation. However, they are not essential. We made use of the material provided by the ichange4health programme, but each province also has its own materials. In the future we should engage more with digital materials, such as the WhatsApp Chatbot. https://pubmed.ncbi.nlm.nih.gov/35537057/
