Implementation
The key aspects of implementation are summarised in the programme theory below.
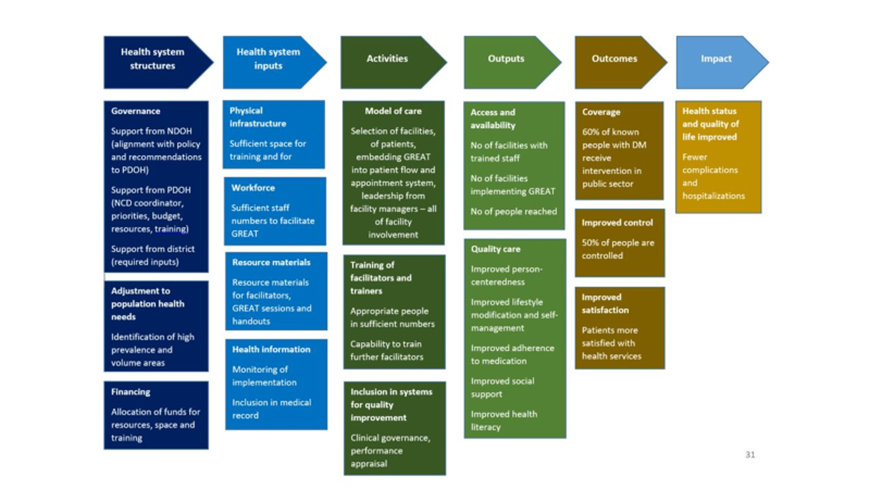
Health system structures
The key policy and decision makers need to support implementation by:
- Making their support visible and the links to policy
- Prioritising implementation in their annual goals and plans
- Funding the costs of implementation
- Supporting the training of facilitators
- Identifying the facilities or key areas for implementation
- Ensuring that the necessary inputs are provided
Health system inputs
Managers need to ensure that the following inputs are in place:
- Suitable space in the facility or local community for groups to meet
- Staff members that can be trained as facilitators
- Availability of the key resource materials, which may have to be printed.
- Monitoring of implementation by the health information system
- Recording of GREAT in patient’s medical records
Activities
Implementing GREAT involves the facility leadership and all those responsible for chronic care. It is not just a matter of training facilitators. A ‘whole of facility’ approach requires visible commitment from the leaders and engagement with staff. For example, the pharmacist may have to fast track dispensing for people in the group, the receptionist may have to pre-draw their folders, the clinicians may have to invite people to attend, and the facilitator will have to be available.
Model of care
Managers and senior clinicians need to think through how GREAT will be embedded in the facility’s processes:
- Who will be trained to facilitate? Usually health promotion officers, nurses or even dieticians. Send the right people for training.
- Who will be targeted? Typically poorly controlled or new patients.
- How will patients be selected or invited? It is better to give people some choice and control.
- How will groups be fitted in to the flow of patients, without disadvantaging those that participate? Don’t make people join the back of the queue afterwards.
- How will attendance at all the sessions be integrated into the appointments that people receive to come back? It is not usually a good idea to make people come for extra visits.
Training of facilitators and trainers
Facilitators are trained in a 3-4 day workshop to understand diabetes, facilitate the groups with a guiding style and use all the resource materials. At least two people per facility should be trained, but more is better.

People need to be developed in each province to train more facilitators. Such training may need to become part of regional training centres and initiatives. These master trainers will be able to train new facilitators for other facilities or to replace facilitators when they move on.
Inclusion in systems for quality improvement
Facilities should monitor the effects of GREAT for diabetes through their own clinical governance systems. Managers should also include the designated activities and responsibilities for their staff in work agreements and performance management.
